Mpox (Monkeypox) Resources
Monkeypox is a rare, viral infection that does not usually cause serious illness. However, it can result in hospitalization or death. That’s why health officials in New York, the U.S., and around the world are monitoring cases of monkeypox in areas that do not usually report monkeypox infections, including in New York State.
On Thursday August 4, 2022, The Biden Administration declared a public health emergency due to the monkeypox outbreak. Everyone should stay informed about monkeypox. This means understanding the symptoms, how it spreads, and what to do if you are exposed. The declaration can be found here.
Vaccination
 Two vaccines are available in the US to prevent monkeypox, but not everyone is eligible to get one.
Two vaccines are available in the US to prevent monkeypox, but not everyone is eligible to get one.
The US has “ample supply” of the smallpox vaccine ACAM2000, which can also be used to prevent monkeypox. However, it shouldn’t be used in people with certain health conditions, according to the CDC.
Another vaccine, Jynneos, is specifically intended for monkeypox, but it’s in short supply. Vaccination with JYNNEOS can be considered for people who are at high risk for infection to prevent monkeypox disease.
Close contacts of someone with monkeypox identified by the Health Department through contact tracing will be offered vaccine for postexposure prophylaxis (PEP). Vaccination within 4 days of an exposure may reduce the chance of monkeypox disease, and vaccination within 5 to 14 days may reduce symptoms.
In addition, a limited amount of vaccine is available to people age 18 or older who may have been recently exposed. Eligibility is currently limited to gay, bisexual, or other men who have sex with men, and/or transgender, gender non-conforming, or gender non-binary who had multiple or anonymous sex partners in the last 14 days.
CDC recommends vaccination for people who have been exposed to monkeypox and people who may be more likely to get monkeypox.
More information about eligibility, current supply, and how to get vaccinated can be found at nyc.gov/monkeypox
Explore nearby healthcare locations providing Monkeypox vaccines via Monkeypox Vaccine Locator | mpoxvaxmap.org
Monkeypox vaccination appointments can be booked online or by calling 877-VAX-4NYC.
Testing
 Consider monkeypox for any patient with a characteristic lesion (deep-seated, well-circumscribed and with central umbilication), or any patient with risk factors and new clinically compatible lesions. The lesions associated with monkeypox characteristically evolve from macules, papules, vesicles, and then pustules, which eventually form scabs that dry and fall off.
Consider monkeypox for any patient with a characteristic lesion (deep-seated, well-circumscribed and with central umbilication), or any patient with risk factors and new clinically compatible lesions. The lesions associated with monkeypox characteristically evolve from macules, papules, vesicles, and then pustules, which eventually form scabs that dry and fall off.
Commercial laboratory testing is now available through LabCorp, Mayo Clinic Laboratories, Aegis Science and Sonic Healthcare. Refer to their websites for lab-specific specimen collection and submission criteria, which may differ among laboratories. Testing offered by Quest Diagnostics has not yet been approved by the NY Clinical Laboratory Evaluation Program and therefore Quest cannot yet accept specimens collected from New York State residents. Providers should submit specimens through commercial laboratories if possible; however, testing will continue to be available at the NYC Public Health Laboratory (PHL) with prior approval by calling the Provider Access Line at 866-692-3641. See Monkeypox Testing at the NYC Public Health Lab on the PHL website for detailed instructions on specimen collection, storage, ordering and transport.
Examination and Diagnosis:
•Collect a complete sexual and travel history for past 21 days
Consider possibility of foreign or domestic animal or animal product contact
•Perform a thorough skin and mucosal examination (e.g., genital, anal, oral) in a room with good lighting
•If rash present, consider a broad differential (e.g., syphilis, varicella zoster, herpes simplex, molluscum contagiosum), especially if the person has epidemiologic risk factors for monkeypox infection in the current outbreak
• Evaluate for STIs per the 2021 CDC STI Treatment Guidelines
Persons with monkeypox have had STIs including acute HIV
Updates on Monkeypox
 Update on Monkeypox in New York City
Update on Monkeypox in New York City
• The number of people in New York City (NYC) diagnosed with monkeypox continues to increase. The latest statistics for monkeypox in New York City can be found here.
• Close, prolonged physical contact including sexual or intimate contact with a person with monkeypox is associated with an increased risk of transmission of the virus among recent cases. While anyone can get monkeypox, almost all of the reported cases are among gay, bisexual, and other men who have sex with men (MSM).
• Testing for monkeypox is now available through LabCorp, Mayo Clinic Laboratories, Aegis Science, and Sonic Healthcare. Providers should submit specimens through commercial laboratories, if possible; however, testing will continue to be available at the NYC Public Health Laboratory with prior approval.
• The JYNNEOSTM vaccine is available through the Health Department for use as expanded postexposure prophylaxis, however supply is very limited.
• Visit the Health Department and Centers for Disease Control and Prevention (CDC) websites for more information about monkeypox.
Update: Monkeypox in New York State – July 2022
As the number of monkeypox cases continues to increase and more local health departments are responding to the outbreak every day, New York State Commissioner of Health Dr. Mary T. Bassett declared monkeypox an Imminent Threat to Public Health (ITPH) in New York State on Thursday, July 28, 2022. The Commissioner’s declaration is pursuant to Public Health Law § 621 and covers monkeypox prevention response and activities undertaken June 1, 2022 through December 31, 2022. Read the Commissioner’s Declaration Letter Here.
The most recent demographic data for monkeypox in New York State can be found here.
Update on Monkeypox From World Health Organization (WHO)
On Saturday, July 23rd, 2022 The World Health Organization declared the monkeypox outbreak a public health emergency of international concern (PHEIC). WHO Director-General Tedros Adhanom Ghebreyesus stated, “I have decided that the global monkeypox outbreak represents a public health emergency of international concern.” Although the committee failed to reach a consensus, Tedros considered the five elements required when deciding whether an outbreak should be declared a public health emergency.
A public health emergency of international concern is defined as “an extraordinary event that constitutes a public health risk to other states through the international spread of disease that may require a coordinated international response. According to the CDC, there are currently 2,800 probable or confirmed cases of monkeypox in the US and Puerto Rico. Monkeypox cases have been reported in 74 countries with over 16,000 cases reported globally. This announcement may incentivize member countries to invest in furthering research and development regarding prevention, treatment, and vaccines.
The WHO Director-General’s Statement can be found here.
Epidemiologic Update
The number of monkeypox cases continues to increase each day. It is important to stay informed about New York City’s monkeypox outbreak. Demographic data can be found here. In reviewing these data, it is important to keep in mind that case detection is impacted by access to care.
Clinical Information
 In the current global outbreak, close, prolonged physical contact including sexual or intimate contact with a person with monkeypox is associated with an increased risk of monkeypox transmission. It is not yet known if people who do not have symptoms can transmit the virus. Atypical features of some cases include a shortened incubation period of 2 to 5 days, the absence of a prodrome, and the presence of only a few, scattered lesions or groups of lesions, often most prominent in the anogenital area. The lesions may involve both skin and mucous membranes. Even with less severe illness, oral, anogenital, or rectal lesions can be very itchy and painful, to the point of interfering with eating, urination, and defecation. Information on transmission and clinical presentation including photos of monkeypox lesions are available on the Centers for Disease Control and Prevention (CDC)’s Clinical Recognition and Clinician FAQs pages.
In the current global outbreak, close, prolonged physical contact including sexual or intimate contact with a person with monkeypox is associated with an increased risk of monkeypox transmission. It is not yet known if people who do not have symptoms can transmit the virus. Atypical features of some cases include a shortened incubation period of 2 to 5 days, the absence of a prodrome, and the presence of only a few, scattered lesions or groups of lesions, often most prominent in the anogenital area. The lesions may involve both skin and mucous membranes. Even with less severe illness, oral, anogenital, or rectal lesions can be very itchy and painful, to the point of interfering with eating, urination, and defecation. Information on transmission and clinical presentation including photos of monkeypox lesions are available on the Centers for Disease Control and Prevention (CDC)’s Clinical Recognition and Clinician FAQs pages.
Causes
Monkeypox is spread when you come into contact with an animal or a person infected with the virus. Animal-to-person transmission occurs through broken skin, like from bites or scratches, or through direct contact with an infected animal’s blood, bodily fluids or pox lesions (sores).
Person to person spread can occur through:
• Direct contact with the infectious rash, scabs, or body fluids
• Respiratory secretions during prolonged, face to face contact, or during intimate physical contact, such as kissing, cuddling, or sex
• Touching items (such as clothing or linens) that previously touched the infectious rash or body fluids
• Through placenta in an infected pregnant person to their fetus
Patients are infectious once symptoms begin (whether prodromal or rash symptoms) and remain infectious until lesions form scabs, scabs fall off, and a fresh layer of skin forms
More information about how monkeypox is spread can be found here.
Signs and Symptoms
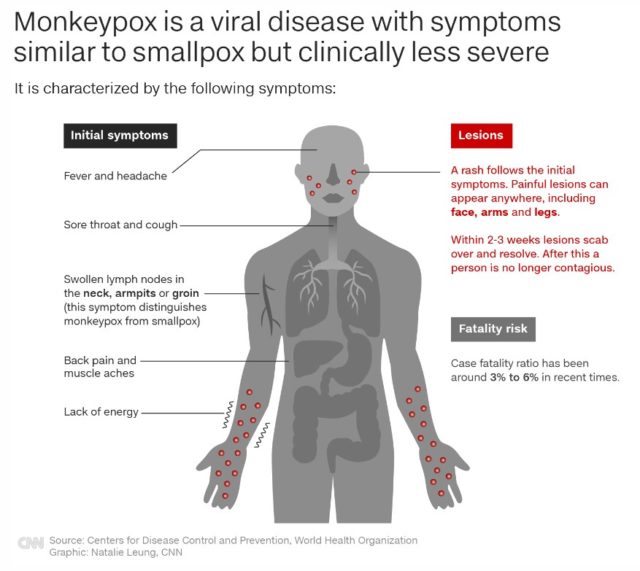 Monkeypox virus is part of the same family of viruses as smallpox. Monkeypox symptoms are similar to smallpox symptoms, but milder; and monkeypox is rarely fatal. Monkeypox is not related to chickenpox.
Monkeypox virus is part of the same family of viruses as smallpox. Monkeypox symptoms are similar to smallpox symptoms, but milder; and monkeypox is rarely fatal. Monkeypox is not related to chickenpox.
Symptoms of monkeypox can include:
• A rash that can look like pimples or blisters that appears on the face, inside the mouth, and on other parts of the body, like the hands, feet, chest, genitals, or anus.
• Chills
• Exhaustion
• Fever
• Headache
• Muscle aches and backache
• Swollen lymph nodes
The rash goes through different stages before healing completely. The illness typically lasts 2-4 weeks. Sometimes, people get a rash first, followed by other symptoms. Others only experience a rash.
The incubation period (interval from infection to onset of symptoms) of monkeypox is usually from 6 to 13 days but can range from 5 to 21 days.
If you experience symptoms, WHO advises that you:
• Avoid scratching your skin
• Keep the skin dry and uncovered
• Clean the skin with sterilized water or antiseptics
• Take a warm bath with baking soda or Epsom salts for lesions on the body
• For lesions in the mouth, use a saltwater rinse like you would for canker sores
CDC guidelines on what to do if you are sick.
More information about the signs and symptoms of monkeypox can be found here.
Treatment
 Most individuals with monkeypox have had a self-limited disease course managed with supportive care. This includes medicines or other clinical interventions to control itching, nausea, vomiting, and pain. Proctitis can occur and though often manageable with appropriate supportive care, can progress to become severe and debilitating which may require prescription medication. Assess the need for and offer appropriate pain management options for each patient; an abundant body of evidence indicates that Black, Latino and other patients of color are less likely to receive sufficient pain management compared to White patients.
Most individuals with monkeypox have had a self-limited disease course managed with supportive care. This includes medicines or other clinical interventions to control itching, nausea, vomiting, and pain. Proctitis can occur and though often manageable with appropriate supportive care, can progress to become severe and debilitating which may require prescription medication. Assess the need for and offer appropriate pain management options for each patient; an abundant body of evidence indicates that Black, Latino and other patients of color are less likely to receive sufficient pain management compared to White patients.
Antiviral treatment with tecovirimat is available via an expanded access investigational new drug (EA-IND) protocol and should be considered for people with severe disease (e.g., sepsis, lesion location or type), illness complications or hospitalization, high risk for severe disease (e.g., severe immunocompromising conditions), risk of stricture or fistula, or significant active exfoliative dermatologic conditions. See the Health Department’s Interim Guidance for Treatment of Monkeypox for detailed guidance regarding supportive treatment and tecovirimat. For information on ordering and prescribing tecovirimat, email [email protected]. Additional guidance on tecovirimat is available from the CDC.
More information on the treatment of monkeypox can be found here.
Prevention
 If you have monkeypox, you are advised to stay at home (isolate) if you have monkeypox symptoms, including until your monkeypox rash has healed and a new layer of skin has formed. Staying away from other people and not sharing things you have touched with others will help prevent the spread of monkeypox. Monkeypox can also spread to animals, so staying away from pets, livestock and other animals is important.
If you have monkeypox, you are advised to stay at home (isolate) if you have monkeypox symptoms, including until your monkeypox rash has healed and a new layer of skin has formed. Staying away from other people and not sharing things you have touched with others will help prevent the spread of monkeypox. Monkeypox can also spread to animals, so staying away from pets, livestock and other animals is important.
• Infection Prevention and Control of Monkeypox in Healthcare Settings
• Monitoring and Risk Assessment for Persons Exposed in the Community
• Notifying Close Contacts
• Preventing Spread to Others
People with monkeypox who do not require hospitalization should be isolated at home. Decisions regarding discontinuation of isolation precautions at a healthcare facility and at home should be made in consultation with the local or state health department.
At this time, the risk of monkeypox to children and adolescents in the United States is low. However, this page answers frequently asked questions about monkeypox for administrators and staff of K-12 schools, early care and education (ECE) programs, camps, and other community settings serving children or adolescents (for example, sports leagues and after-school programs).
Patients waiting for test results are advised to isolate at home, avoid contact with others, and monitor their symptoms. If the test result is positive, advise them to continue to follow the same precautions until all scabs have fallen off and a fresh layer of skin has formed. This can take two to four weeks from when the rashes or lesions first appear. See CDC guidelines for precautions that should be taken to decrease the risk of transmitting monkeypox to others.
Complications
Monkeypox typically presents clinically with fever, rash and swollen lymph nodes and may lead to a range of medical complications. Complications include:
• Bronchopneumonia
• Corneal infection with ensuing visual loss
• Encephalitis
• Secondary skin infection
• Sepsis
If the patient is pregnant, there may be complications, including preterm delivery, fetal death, or congenital disease. Mortality has historically ranged from 0-10%. Only three previous outbreaks have occurred:
• Central Africa 1996-1998, mortality ~10%
• USA 2003, mortality 0%
• Nigeria 2017-present (~200 confirmed cases), mortality 3%
More information about monkeypox complications can be found here.
Outbreaks
 Human monkeypox was first identified in humans in 1970 in the Democratic Republic of the Congo in a 9-month-old boy in a region where smallpox had been eliminated in 1968. Since then, most cases have been reported from rural, rainforest regions of the Congo Basin, particularly in the Democratic Republic of the Congo and human cases have increasingly been reported from across central and west Africa.
Human monkeypox was first identified in humans in 1970 in the Democratic Republic of the Congo in a 9-month-old boy in a region where smallpox had been eliminated in 1968. Since then, most cases have been reported from rural, rainforest regions of the Congo Basin, particularly in the Democratic Republic of the Congo and human cases have increasingly been reported from across central and west Africa.
Since 1970, human cases of monkeypox have been reported in 11 African countries: Benin, Cameroon, the Central African Republic, the Democratic Republic of the Congo, Gabon, Cote d’Ivoire, Liberia, Nigeria, the Republic of the Congo, Sierra Leone and South Sudan. Since 2017, Nigeria has experienced a large outbreak, with over 500 suspected cases and over 200 confirmed cases and a case fatality ratio of approximately 3%. Cases continue to be reported until today.
In 2003, the first monkeypox outbreak outside of Africa was in the United States of America and was linked to contact with infected pet prairie dogs. This outbreak led to over 70 cases of monkeypox in the U.S. Monkeypox has also been reported in travelers from Nigeria to Israel in September 2018, to the United Kingdom in September 2018, December 2019, May 2021 and May 2022, to Singapore in May 2019, and to the United States of America in July and November 2021. In May 2022, multiple cases of monkeypox were identified in several non-endemic countries. Studies are currently underway to further understand the epidemiology, sources of infection, and transmission patterns.
More information on previous monkeypox outbreaks can be found here.
Reporting and Assistance
Clinicians should first consult their state health department (State Contacts) as soon as monkeypox is suspected. If you have a patient that meets the probable or confirmed case definition, the health department will contact the CDC Monkeypox Call Center at [email protected] to report the case and fill out the case report form.
Support
 We acknowledge the hardships associated with caring for someone with a new disease that is time-consuming to diagnose. This is in addition to the ongoing COVID-19 pandemic and distressing news about current events. NYC WELL continues to be a resource for you, your patients, and all New Yorkers.
We acknowledge the hardships associated with caring for someone with a new disease that is time-consuming to diagnose. This is in addition to the ongoing COVID-19 pandemic and distressing news about current events. NYC WELL continues to be a resource for you, your patients, and all New Yorkers.
For any mental health support, NYC Well is the connection to free, confidential crisis counseling, mental health and substance use support, information and referrals. The help line is available 24 hours a day, 7 days a week by calling 888-NYC-WELL (888-692-9355), texting WELL to 65173, and online chat.
Stigma
 Numerous cases are occurring in the gay, bisexual, and other men who have sex with men (MSM) community, leaving many concerned about increased stigma. How can scientists communicate about monkeypox without stirring discrimination or panic?
Numerous cases are occurring in the gay, bisexual, and other men who have sex with men (MSM) community, leaving many concerned about increased stigma. How can scientists communicate about monkeypox without stirring discrimination or panic?
All kinds of sexual contact are intimate contact by definition. It could be heterosexual contact, it could be MSM contact. Often, outbreaks get identified in certain communities, but that doesn’t mean that one specific type of sexual behavior is inherently more conducive to the transmission. An at-risk community gets identified because someone from that community travelled somewhere and started an outbreak. It’s a situation that occurs because of the intimacy of the contact, not the kind of sex people are having.
CDC’s response in reducing stigma in monkeypox communication and community engagement
Helpful Links
• Monkeypox Vaccine Locator | mpoxvaxmap.org
• U.S. Monkeypox 2022: Situation Summary
• 2022 U.S. Map & Case Count
• Monkeypox (Español)
• CDC’s Response to the 2022 Monkeypox Outbreak
• Vaccines
• Safer Sex, Social Gatherings, and Monkeypox
• Reducing Stigma in Monkeypox Communication and Community Engagement
• Videos
• Print Resources
More Resources
• CDC-7 Questions on Monkeypox Video
• CDC- Considerations for Monkeypox Vaccination
• CDC- Disinfecting Home and Other Non-Healthcare Settings
• CDC- Monkeypox Fact Sheet
• CDC- Monkeypox FAQs
• CDC- Smallpox/Monkeypox Vaccine Information Statements
• Clinician FAQs
• Duration of Isolation Procedures
• How to Safely Wash Your Laundry if You Have Monkeypox
• Infection Prevention and Control of Monkeypox in Healthcare Settings
• JYNNEOS Vaccine for Monkeypox: Frequently Asked Questions
• Monkeypox Myths – USA Today
• Monkeypox Travel Notice
• Monkeypox Virus – Interim Fact Sheet
• NYC Department of Health Daily Monkeypox Data
• NYC Department of Health Monkeypox Page
• NYC Health Map
• NYC Smallpox/Monkeypox Vaccine Appointment Scheduler
• New York State Department of Health- Monkeypox
• Preventing Monkeypox Spread in Specific Settings
• Pan American Health Organization Monkeypox Q&A
• Reducing Stigma in Monkeypox Communication and Community Engagement
• What to Expect After Your Monkeypox Vaccine
• WHO Monkeypox Information Page
• New Yorkers can sign-up for monkeypox text alerts from New York State by texting “MONKEYPOX” to 81336 or “MONKEYPOXESP” for texts in Spanish. By providing a zip code, New Yorkers can also opt-in for location-based messages, which may include information on vaccines and care in your area.
• To get text alerts about vaccination appointments and other monkeypox updates for NYC, text “MONKEYPOX” to 692-692.
• Monkeypox vaccination appointments can be booked online or by calling 877-VAX-4NYC.